Post operative chest
- 1. POST OPERATIVE CHEST 23-12-2015 Dr.Y. Madhu Madhava Reddy
- 2. Introduction Intrathoracic surgery is performed most frequently for resection of all or part of lung, or for cardiac disease. So it is must for a radiologist to have the knowledge of acute and chronic radiological appearances of such surgical conditions and their complications.
- 3. Thoracotomy Lung resections are usually performed posterolaterally through the 4th or 5th intercostal space. Part of rib may be resected, the periosteum may be stripped or ribs may simply be spread apart following a muscle incision. Surgical route is not obviously identified on Chest X ray, or is marked only by some narrowing of Intercostal space / overlying soft tissue swelling and Sub cuteneous emphysema.
- 4. RIBS
- 6. Pneumonectomy It is important for remaining lung to be fully expanded following pneumonectomy, and for mediastinum to remain close to the midline. Excessive mediastinal shift may compromise respiration and venous return to the heart. Initial post op CXR, the trachea should be close to midline, the remaining lung should appear normal or slightly Plethoric.
- 7. Pneumonectomy space also usually contain small amount of fluid initially, and this space begins to obliterate by gradual shift of mediastinum to that side and accumulation of fluid. If the mediastinum moves towards the opposite side, this may indicate rapid accumulation of fluid in pneumonectomy space or atelectasis in remaining lung. A sudden shift may indicate Bronchopleural fistula.
- 8. Day 1 Day 6 5 weeks 8 weeks
- 9. Day 2Day 1 Day 14 Day 30
- 10. Following Lobectomy Remaining lung should expand to fill space of resected lobe. Immediately Post operatively, pleural drains are present, preventing accumulation of pleural fluid, and mediastinum may be shifted to the side of operation. With hyperinflation of the remaining lung the mediastinum returns to its normal position.
- 11. Following Segemental / Subsegmental resection A cut surface of lung is oversewn, and air leaks are common, sometimes causing persistent pneumothorax which may require prolonged drainage. Wire sutures or staples may be visible at the site of bronchial stump or lesser lung resections.
- 12. Complications of Thoracotomy Postoperative spaces Empeyma Bronchopleural fistula Pleural fluid Diaphragmatic elevation
- 13. Postoperative spaces These may persist following lobectomy and segmental or subsegmental resections. There are the air spaces that correspond to the excised lung. Fluid may collect in them, they usually resolve after few weeks or months. If they persist, they may cause an empyema or bronchopleural fistula.
- 14. Empyema It usually occurs a few weeks after surgery, it may occur few months or years later. Rapid accumulation of fluid may cause mediastinal shift to normal side. If a fistula develops between the pneumonectomy space and a bronchus or skin, the air fluid level in the space will suddenly drop.
- 15. Empyema
- 16. Bronchopleural Fistula This is communication between bronchial tree or lung tissue and pleural space. The commonest cause of this is a lung surgery. It can be resulted from rupture of a lung abscess, erosion by a lung cancer or penetrating trauma. BPF complicating complete or partial lung resection may occur early, when it is due to faulty closure of bronchus. But it commonly occurs late due to infection or tumour of the bronchial stump.
- 17. Radiographic appearance is sudden appearance of, or increase in the amount of air in the pleural space, with a corresponding decrease in the amount of fluid in the space. If fluid enters airways and is aspirated into the remaining lung, widespread consolidation is seen. Sinography of pleural space or bronchography may demonstrate the fistula.
- 20. Esophagopleural fistula 2 yrs post-op
- 22. Pleural fluid Usually seen on CXR following thoracic surgery. If the amount is excessive it may be due to bleeding or chylothorax.
- 23. Diaphragmatic elevation Elevation may indicate phrenic nerve damage and is best assessed by fluoroscopy or ultrasound.
- 24. Cardiac surgery Most of them are performed through a sternotomy incision and wire sternal sutures are often seen on postoperative films. Following cardiac surgery, some widening of the cadiovascular silhouette is usual, and represents bleeding and oedema. Marked mediastinal widening suggests significant haemorrhage.
- 25. Some air remains in pericardium following cardiac surgery. Pulmonary opacities are very common following open heart surgery, and left basal shadowing is almost invariable, indicating atelectasis. Small pleural effusions are also common in immediate post op period.
- 26. Haemorrhage following cardiac transplantation 4hrs postop After chest tube insertion
- 28. Pneumoperitoneum is sometimes seen due to involvement of peritoneum by sternotomy incision. Violation of left or right pleural space may lead to chylothorax or more localised collection, a chylonur. Phrenic nerve damage cause paresis or paralysis of hemidiaphragm.
- 29. Prosthetic heart valves are usually visible of CXR. Surgical clips or other metallic markers have sometimes been used to mark ends of coronary artery bypass grafts.
- 30. Heart valves
- 31. Sternal dehiscence appears radiographically as a linear lucency appearing in sternum and alteration in position of the sternal sutures. It may be associated with osteomyelitis. Fractures of 1st or 2nd rib occur when the sternum is spread apart, and they explain the chest pain in postoperative period.
- 32. Acute mediastinitis can occur as complication or surgery. It is more commonly associated with esophageal perforation or surgery. Radiographically there will be mediastinal widening or pneumomediastinum.
- 34. Chronic mediastinal infection – includes sternal osteomyelitis may occur after median sternotomy. Increasing amounts of gas in mediastinum on subsequent examination is indicative of the presence of a gas forming organism.
- 37. The postpericardotomy syndrome is an autoimmune phenomenon, usually occuring in the month after surgery. It presents with fever, pleurisy, and pericarditis. Pleural effusions and cardiomegaly may be present on CXR. Ultrasound demonstrate pericardial fluid. Patchy consolidation may occur in lung bases.
- 38. Late appearances after chest surgery Resected ribs, healed rib fractures are frequently seen, there may be irregular regeneration of rib related to disturbed periosteum. Rearrangement of remaining lung occurs after lobectomy, causing alteration in anatomy of fissures.
- 40. Following esophageal surgery, stomach or loops of bowel may produce unusual soft tissue opacities or fluid levels if they have been brought up into chest.
- 42. Misc. Surgery for Pulmonary tuberculosis is now rarely performed. The objective of surgery was to reduce aeration to infected lung, usually upper lobe. Thoracoplasty is combined with pneumonectomy for treatment of Chronic tuberculous empyema.
- 43. Alternative method was, Plombage, which was the extrapleural insertion of some inert material to collapse the underlying lung. Solid or hollow Incite balls were commonly used. Other substances incluse crumpled cellophane packs and paraffin.
- 44. Plombage
- 45. Oleothorax
- 46. Ping pong ball plombage
- 47. Thoracic complications of General surgery Atelectasis Pleural effusions Pneumothorax Aspiration pneumonitis Pulmonary edema Pneumonia Subphrenic abscess Pulmonary embolism
- 48. Atelectasis Commonest after thoracic or abdominal surgery. Predisposing factors: long anaesthetic, obesity, chr. Lung disease and smoking. It results form retained secretions and poor ventilation. Postoperatively it is painful to breathe deeply or cough. CXR findings: elevation of diaphragm due to poor inspiration. Lower zone opacities representing subsegmental volume loss and consolidation (appear at 24hrs- resolve by 2- 3days).
- 49. Pleural effusions Occur immediately following abdominal surgery and resolve in 2 weeks. May be associated with pulmonary infarction. Effusions due to sub phrenic infection usually occur later.
- 50. Pneumothorax When it complicates extrathoracic surgery, it is a complication of positive pressure ventilation or central venous line insertion. It may complicate nephrectomy.
- 51. Aspiration pneumonitis It is common during anaesthesia but insignificant. When significant, patchy consolidation appears within a few hours, usually basally or around the hila. Clearing occurs within few days, unless there is super added infection.
- 53. Pulmonary edema It be may due to cardiogenic or non- cardiogenic. Non-cardiogenic includes fluid overload and the adult respiratory distress syndrome.
- 54. Pneumonia Post op atelectasis and aspiration pneumonitis may be complicated by pneumonia. They tend to be associated with bilateral basal shadowing.
- 55. Subphrenic abscess It produces elevation of hemidiaphragm, pleural effusion and basal atelectasis. Loculated gas may be seen below diaphragm and fluoroscopy may show splinting of diaphragm. It can be demonstrated by ct or ultrasound.
- 56. Pulmonary embolism It produces pulmonary shadowing, pleural effusion or elevation of diaphragm. Normal chest radiograph does not exclude pulmonary embolism. So initial investigation is perfusion lung scan.
- 57. Patient in ICU Patients are shifted to an intensive care unit post operatively, following major trauma or circulatory or respiratory failure. A number of monitoring and life support devices are used. Radiology plays an important role in management of these devices.
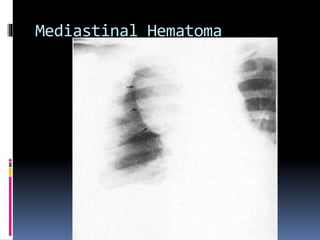
- 58. CVP catheters Used to monitor RA pressure. One end of CVP line needs to be intrathoracic, ideally in SVC. Subclavian approach for their insertion carries a risk of pneumothorax and mediastinal hematoma. Catheters have potential risk of coiling, knotting or fracture leading to embolism.
- 61. Pneumothorax
- 62. Swan-Ganz catheters Used to measure pulmonary artery and pulmonary wedge pressures(indicator of LA pressure). Introduced via antecubital vein / jugular vein. Inflatable balloon at the tip guides it through the right heart. End of catheter should be maintained 5-8cms beyond bifurcation of Main pul. artery in either LA or RA.
- 63. When wedge pressure is measured, balloon is inflated and flow of blood carries the catheter tip peripherally, to a wedge position. After measurement, balloon is deflated and catheter returns to a central position, otherwise there is a risk of pulmonary infarction.
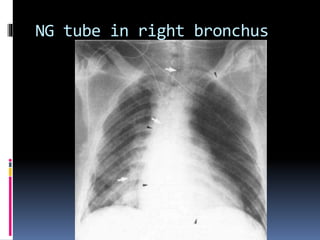
- 64. NG tube These may not reach stomach or may coil in esophagus or occasionally are inserted into trachea and into right bronchus.
- 65. NG tube in right bronchus
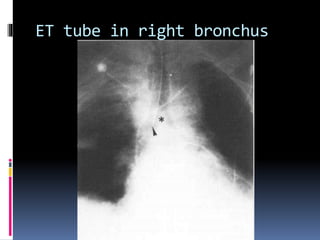
- 66. Endotracheal tubes Used to access airways for ventilation and management of secretions, and also protect airway. CXR is essential in assessig position of tip of ET tube relative to carina. Neck extension and flexion make tip of ET tube move by 5cms. With neck in neutral position the tip of ET tube should ideally be about 5-6cms above carina.
- 67. Tube that is inserted too far usually passess into the right bronchus with risk of collapse of left lung. If inflated cuff dilate trachea, there is risk of ischaemic damage to tracheal mucosa. Late complication of over inflatted cuff is tracheostenosis.
- 68. ET tube in right bronchus
- 69. Tracheostomy tubes Used for long term ventillatory support. Tube tip should be situated centrally in airway at the level ofT3. Acute complications of tracheostomy include pneumothorax, pneumomediastinum and sub cuteneous emphysema. Long term complications include tracheal ulceration, stenosis and perforation.
- 70. Positive pressure ventilation Complications may include: Interstitial emphysema Pneumomediastinum Pneumothorax Sub cuteneous emphysema
- 71. Pleural tubes Used to treat pleural effusion and pneumothoraces. If patient is being nursed supine, tip of tube should be placed anteriorly and superiorly for a pneumothorax and posteriorly and inferiorly for an effusion. A radio opaque line runs along the tubes and interrupted where there are side holes. It is important to check all side holes are in thorax.
- 72. Pneumothorax
- 73. Mediastinal drains Apart from their position they looks like pleural tubes. These are usually present following sternotomy.
- 74. Intra-aortic balloon pump IABP is a long balloon temporary circulatory device that works on the principle of cardiac counter pulsation. IABP is used to support circulation. The balloon, approximately 25cms long, is mounted on a catheter. The catheter tip is visible as a 3x4mm rectangular metallic density, rest of catheter is radiolucent.
- 75. Catheter is inserted through femoral artery. The balloon is inflated with gas during diastole and deflates during systole, resulting in increase in coronary blood flow and reduction in left ventricular afterload( and hence, reduction in myocardial oxygen consumption). Indications: MI with cardiogenic shock, post coronary by pass graft, acute mitral insufficiency and cardiac transplantation.
- 76. IABP
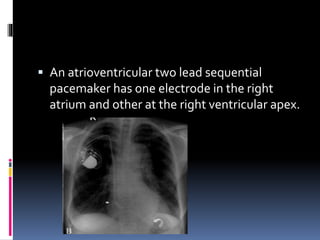
- 77. Pace makers Used in cases of severe sinus node dysfunction, complete heart block and various arrythmias. 2 main elements: pulse generator and lead wire with electrodes. Single lead pacemaker is most basic type and is positioned with its tip in the right ventricular apex.
- 79. An atrioventricular two lead sequential pacemaker has one electrode in the right atrium and other at the right ventricular apex.
- 80. The potential complications are malposition, intracardiac knotting , fracture, perforation
- 81. Transplantations Cardio pulmonary transplantations are uncommon procedures, with only a few thousand cases undertaken worldwide each year. Heart transplant remains most frequent procedure.
- 82. Heart transplantation Basal atelectasis especially in left lower lobe. Small effusions Haematoma within pleura or mediastinum. Chest drains are places during surgery, pneumothorax and pneumomediastinum are frequent. Pneumoperitoneum is seen in immediate postop period.
- 83. Pulmonary edema is seen if cardiac function depresses in post op period. Complications related to rejection are usually manifest by cardiac failure. Rejection may be acute , within 3 months, or chronic in subsequent months or years. Specific complication of heart transplantation is accelerated coronary artery disease. Long term immune suppression to prevent rejection- increased risk of lymphoma.
- 84. Lymphoma postop 2 months
- 85. Lung transplant Low success rate. Single lung transplantation is preferred over double lung transplantation. Radiology plays role in multidisciplinary approach of donor selection, particularly in excluding occult contraindications like lung tumours / infections in opposite lung and assessment of degree and extent of pleural abnormality.
- 86. Complications Acute phase: reperfusion edema due to prolonged ischemia resulting in increased capillary permiability. Duration and severity of reimplantation response is reduced by minimising ischaemic time and careful restriction of postop fluid replacement.
- 87. Acute rejection: occur after 5th post op day. CXR may be normal or may demonstrate diffuse interstitial edema with pleural effusion. Infections complicate postoperative period. Colonisation of upper airway by virulent hospital flora, impaired clearance of nasopharyngeal secretions, immune suppression theraphy, impairment of mucociliary escalator are factors of infection.
- 88. Anastomotic failures, occasionally vascular but more frequently bronchial, may result in dehiscence or stenosis. Bronchial dehiscence may cause mediastinal emphysema, confirmed by CT, by identifying bronchial wall defect. Late rejections commonly manifest as bronchiolitis obliterans, confirmed by HRCT, demonstrates variation in attenuation of parenchyma(air trapping).
- 90. Thank you
Editor's Notes
- #5: Rib defect following thoracotomy for right upper lobe Ca. Late postsurgical changes following periosteal stripping for mitral valvotomy.
- #10: Normal postoperative anatomy at chest radiography in a 55-year-old man who underwent left pneumonectomy for squamous cell carcinoma. (a) Radiograph on postoperative day 1 shows pneumothorax in the postpneumonectomy space, a midline trachea, and slight congestion in the remaining right lung. (b) Radiograph on postoperative day 2 shows fluid in the lower one-third of the postpneumonectomy space. (c) Radiograph on postoperative day 14 shows that the air-fluid level has risen in the postpneumonectomy space. (d) Radiograph on postoperative day 30 shows total opacification of the postpneumonectomy space and elevation of the left hemidiaphragm.
- #16: Empyema in a 74-year-old man after left pneumonectomy for sarcomatoid carcinoma. (a) Chest radiograph on postoperative day 21 shows a midline position of the trachea, mediastinum, and tracheostomy tube and total opacification of the postpneumonectomy space. (b) Chest radiograph on postoperative day 50 shows a rightward deviation of the trachea with tracheostomy tube and of the mediastinum because of overexpansion of the postpneumonectomy space. (c) Axial CT image on postoperative day 52 shows irregular pleural thickening in the postpneumonectomy space and an abscess (arrow) in the posterior chest wall, findings suggestive of empyema. A chest tube was inserted for drainage
- #19: Thirteen days after right pneumonectomy the space is filling with fluid and the mediastinum is deviated to the right. (B) Two days later, after the patient coughed up a large amount of fluid, the fluid level has dropped and the mediastinum has returned to the midline. Bronchoscopy confirmed a right bronchopleural fistula.
- #20: Bronchopleural fistula in a 65-year-old man after right pneumonectomy for large cell carcinoma. (a) Chest radiograph on postoperative day 18 shows near complete opacification of the postpneumonectomy space. (b) Chest radiograph on postoperative day 20 shows recurrent air-fluid levels in the middle of the postpneumonectomy space. (c) Chest radiograph on postoperative day 22 shows tension pneumothorax, subcutaneous emphysema (*), and a leftward shift of mediastinal structures, including the trachea. A chest tube subsequently was inserted for drainage. (d) Axial CT image demonstrates a fistula (arrow
- #21: Esophagopleural fistula in a 53-year-old man after right pneumonectomy for squamous cell carcinoma. (a) Chest radiograph 2 years after pneumonectomy shows a recurrent air- fluid level (arrow) in the postpneumonectomy space. (b) Axial CT image demonstrates a fistula between the esophagus and the postpneumonectomy space (arrowhead). (c) Esophagogram shows leakage of oral contrast material through the esophagopleural fistula (arrow)
- #22: Recurrent tumor in a 39-year-old man after left pneumonectomy for squamous cell carcinoma. (a) Chest radiograph shows segmental consolidation that was presumed to be due to aspiration pneumonia in the lower lobe of the right lung. (b) Esophagram shows a thin linear area of contrast material (arrow) that has leaked from the esophagus at the level of the carina. (c) Coronal CT image depicts a necrotic lymph node, which is indicative of recurrent metastatic carcinoma, and a resultant esophago-nodo-bronchial fistula at the carina.
- #27: Haemorrhage following cardiac transplantation. (A) Four hours following return from surgery the chest radiograph reveals opacification of the right upper zone. Ultrasound at the patient's bedside confirmed a large fluid collection. (B) After insertion of a chest drain there has been partial resolution of the appearances.
- #28: Enhanced CT scan demonstrates a soft-tissue density non-enhancing mass in the anterior mediastinum 3 days following cardiac surgery
- #34: Small retrosternal air fluid collection., enlarged azygous vein d/t previous thrombosis of SVC. Infected mediastinal collection after ASD closure.
- #36: Post esophagectomy., collection., B/l pl eff. Drainage ct guided by pig tail catheter in pt semiprone position.
- #37: Haemopneumopericardium after 2 days closure of ASD. White arrows..air outlining., fluid level (black arrowheads)., B/l Pl effusions.
- #40: Right side: repair of TEFistula., rib defect present Left side: Pair of VSD., thoracotomy wound sealing done., so IC space decreased
- #42: a.Oesophagectomy., there is rib defect., air under rt dome., gastric conduit in rt chest. B. Dilated gastric pull up., air fluid level seen in distended conduit in left chest d/t gastric out flow obstruction
- #45: Several hollow balls inserted extrapleurally in left apex. Ct in another patient, lucite balls in rt apex
- #46: Oleothorax. Plombage has been performed by instilling kerosene (paraffin) extrapleurally through a thoracotomy with excision of the fifth rib. A thin rim of calcification has developed in the extrapleural collection. Some keresone has tracked inferiorly behind the lung and produced a calcified pleural plaque which is seen en face (arrowheads).
- #53: 6hrs after intubation., b/l basal and perihilar air space shadowing due to aspiration of gastric contents. Swan ganz catheter insitu.
- #60: Following unsuccessful attempt of CVP placing via rt subclavian vein... Large hematoma.
- #61: Cvp catheter introduced via left jug vein. It points inferiorly rather than along axis of innominate vein. Pl eff present. Contrast via catheter demons. Extravasatn and comm with pl eff.
- #73: Chest tube entering lung parenchyma. Extensive parenchymal changes due to ARDS and rt sided pul haematomas.