Rectal Cancer
- 1. CA Rectum Presented By: Dr. MONSIF IQBAL Dept. of Surgery POF Hospital, Wah Cantt, Pakistan
- 3. PATIENT’s PROFILE: • Name: XYZ • Age: 60 yrs. • Sex: Male • Address : Islamabad. • D.O.A: 04-09-2013 • M.O.A: OPD
- 4. PRESENTING COMPLAINTS • Constipation 1.5 years • Bleeding PR 6 months • Diagnosed case of CA Rectum
- 5. Past History Sigmoidoscopy done in POF Hospital, Adenocarcinoma Rectum (March--April 2013)
- 6. Past History Cont. CT Scan Abdomen+Pelvis was done (April 2013)
- 7. Past History Cont. • Neo-adjuvant Chemotheray and radiotherapy in PIMS and Nescom Hospital
- 8. PHYSICAL EXAMINATION: On Examination ▫ Pulse: 92/min ▫ B.P: 135/70 mm of Hg ▫ Oxygen Sat: 99% On Abdominal Examination Distended Non tender
- 9. INVESTIGATIONS 1. Blood CP: • Hb ---- 11.3 gm/dl • TLC ---- 11.6x103 /ul • PLT ---- 434x103 /ul 2. ALT: 57 3. RFTs: Urea: 34, Creatinine 0.75 sodium : 139 Potassium : 4.0 Chloride : 101 4. CEA : 125
- 10. CT Scan Abdomen+Pelvis was done (Sep 2013)
- 11. Management • IV fluids • IV antibiotics and Analgesics started • Councelled for APR • Planned APR
- 19. CA Rectum
- 20. Clinical Anatomy • 12-15 cm from anal verge. • Diameter ▫ 4 cm (upper part) ▫ Dilated (lower part) • Posterior part of the lesser pelvis and in front of lower three pieces of sacrum and the coccyx • Begins at the rectosigmoid junction, at level of third sacral vertebra • Ends at the anorectal junction, 2-3 cm in front of and a little below the coccyx
- 21. • Divided into 3 parts • Upper third • Middle third • Lower third • 3 distinct intraluminal curves ( Valves of Houston)
- 22. • Superior 1/3rd of the rectum ▫ Covered by peritoneum on the anterior and lateral surfaces • Middle 1/3rd of the rectum ▫ Covered by peritoneum on the anterior surface • Inferior 1/3rd of the rectum ▫ Devoid of peritoneum ▫ Close proximity to adjacent structure including boney pelvis. Peritoneal Relations
- 23. Arterial supply • Superior rectal A – fr. IMA; supplies upper rectum • Middle rectal A- fr. Internal iliac A. (supplies middle rectum) • Inferior rectal A- fr. Internal pudendal A. supplies lower rectum Venous drainage ▫ Superior rectal V- upper & middle third rectum ▫ Middle rectal V- lower rectum and upper anal canal ▫ Inferior rectal vein- lower anal canal Innervations • Sympathetic: L1-L3, Hypogastric nerve • ParaSympathetic: S2-S4
- 24. Lymphatic drainage • Upper and middle rectum ▫ Pararectal lymph nodes, located directly on the muscle layer of the rectum ▫ Inferior mesenteric lymph nodes, via the nodes along the superior rectal vessels • Lower rectum ▫ Sacral group of lymph nodes or Internal iliac lymph nodes • Below the dentate line ▫ Inguinal nodes and external iliac chain
- 25. Epidemiology • Colorectal caner is the third most frequently diagnosed cancer in the US men and women. • 108,070 new cases of colon cancer and 40,740 new cases of rectal cancer in the US in 2008. Combined mortality for colorectal cancer 49,960 in 2008. • Worldwide approx. 1 million new cases p.a. are diagnosed, with 529,000 deaths. • Incidence rate in India is quite low about 2 to 8 per 100,000 • Incidence in Wah Cantt, Taxilla and surrounding Sub-urban areas is 55---60 cases per year. • Median age- 7th decade but can occur any time in adulthood.
- 26. • Cecum 14 % • Ascending colon 10 % • Transverse colon 12 % • Descending colon 7 % • Sigmoid colon 25 % • Rectosigmoid junct 0.9 % • Rectum 23 %
- 27. Etiological agents Environmental & dietary factors Chemical carcinogenesis. Associated risk factors Male Gender Family history of colorectal cancer Personal history of colorectal cancer, ovary, endometrial, breast Excessive BMI Processed meat intake Excessive alcohol intake Low folate consumption Neoplastic polyps. Hereditary Conditions (FAP, HNPCC)
- 28. Clinical Presentations • Symptoms ▫ Asymptomatic ▫ Change in bowel habit (diarrhoea, constipation, narrow stool, incomplete evacuation, tenesmus). ▫ Blood PR. ▫ Abdominal discomfort (pain, fullness, cramps, bloating, vomiting). ▫ Weight loss, tiredness. • Acute Presentations ▫ Intestinal obstruction. ▫ Perforation. ▫ Massive bleeding.
- 29. • Signs ▫ Pallor ▫ Abdominal mass ▫ PR mass ▫ Jaundice ▫ Nodular liver ▫ Ascites
- 30. Pathological features WHO Classification • Adenocarcinoma in situ • Adenocarcinoma • Mucinous (colloid) adenocarcinoma (>50% mucinous) • Signet ring cell carcinoma (>50% signet ring cells) • Squamous cell (epidermoid) carcinoma • Adenosquamous carcinoma • Small-cell (oat cell) carcinoma • Medullary carcinoma • Undifferentiated Carcinoma
- 31. Dukes classification- Dukes A: Invasion into but not through the bowel wall. Dukes B: Invasion through the bowel wall but not involving lymph nodes. Dukes C: Involvement of lymph nodes Dukes D: Widespread metastases Modified astler coller classification- Stage A : Limited to mucosa. Stage B1 : Extending into muscularis propria but not penetrating through it; nodes not involved. Stage B2 : Penetrating through muscularis propria; nodes not involved Stage C1 : Extending into muscularis propria but not penetrating through it. Nodes involved Stage C2 : Penetrating through muscularis propria. Nodes involved Stage D: Distant metastatic spread
- 32. Tis TTis T11 TT22 TT33 TT44 MucosaMucosa Muscularis mucosaeMuscularis mucosae SubmucosaSubmucosa Muscularis propriaMuscularis propria SubserosaSubserosa SerosaSerosa TNM Classification TX Primary tumor cannot be assessed T0 No evidence of primary tumor Tis Carcinoma in situ: intraepithelial or invasion of lamina propria T1 Tumor invades submucosa T2 Tumor invades muscularis propria T3 Tumor invades through the muscularis propria into pericolorectal tissues T4a Tumor penetrates to the surface of the visceral peritoneum T4b Tumor directly invades or is adherent to other organs or structures
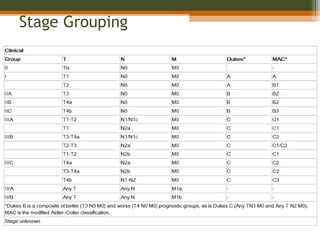
- 34. Stage Grouping
- 35. Prognostic factors Good prognostic factors Old age Gender(F>M) Asymptomatic pts Polypoidal lesions Diploid Poor prognostic factors Obstruction Perforation Ulcerative lesion Adjacent structures involvement Positive margins LVSI Signet cell carcinoma High CEA Tethered and fixed cancer
- 36. Stage and Prognosis Stage 5-year Survival (%) 0,1 Tis,T1;No;Mo > 90 I T2;No;Mo 80-85 II T3-4;No;Mo 70-75 III T2;N1-3;Mo 70-75 III T3;N1-3;Mo 50-65 III T4;N1-2;Mo 25-45 IV M1 <3
- 37. Diagnostic Workup • History—including family history of colorectal cancer or polyps • Physical examinations including DRE and complete pelvic examination in women: size, location, ulceration, mobile vs. tethered vs. fixed, distance from anal verge and sphincter functions. • Proctoscopy—including assessment of mobility, minimum diameter of the lumen, and distance from the anal verge • Biopsy of the primary tumor
- 38. Colonoscopy or barium enema Figure: Carcinoma of the rectum. Double- contrast barium enema shows a long segment of concentric luminal narrowing (arrows) along the rectum with minimal irregularity of the mucosal surface. To evaluate remainder of large bowel to rule out synchronous tumor or presence of polyp syndrome.
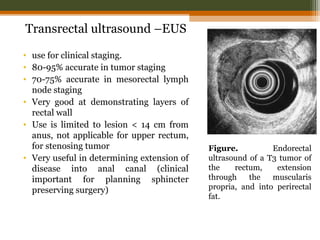
- 39. Transrectal ultrasound –EUS • use for clinical staging. • 80-95% accurate in tumor staging • 70-75% accurate in mesorectal lymph node staging • Very good at demonstrating layers of rectal wall • Use is limited to lesion < 14 cm from anus, not applicable for upper rectum, for stenosing tumor • Very useful in determining extension of disease into anal canal (clinical important for planning sphincter preserving surgery) Figure. Endorectal ultrasound of a T3 tumor of the rectum, extension through the muscularis propria, and into perirectal fat.
- 40. CT scan • Part of routine workup of patients • Useful in identifying enlarged pelvic lymph-nodes and metastasis outside the pelvis than the extent or stage of primary tumor • Limited utility in small primary cancer • Sensitivity 50-80% • Specificity 30-80% • Ability to detect pelvic and para-aortic lymph nodes is higher than peri-rectal lymph nodes.
- 41. Magnetic Resonance Imaging (MRI) • Greater accuracy in defining extent of rectal cancer extension and also location & stage of tumor • Also helpful in lateral extension of disease, critical in predicting circumferential margin for surgical excision. • Different approaches (body coils, endorectal MRI & phased array technique)
- 42. Figure: Mucinous adenocarcinoma of the rectum. T2-weighted MRI shows high signal intensity (arrowheads) of the cancer lesion in right anterolateral side of the rectal wall. Figure: Normal rectal and perirectal anatomy on high-resolution T2-weighted MRI. Rectal mucosa (M), submucosa (SM), and muscularis propria (PM) are well discriminated. Mesorectal fascia appears as a thin, low-signal-intensity structure (arrowheads) and fuses with the remnant of urogenital septum making Denonvilliers fascia (arrows).
- 43. PET • Shows promise as the most sensitive study for the detection of metastatic disease in the liver and elsewhere. • Sensitivity of 97% and specificity of 76% in evaluating for recurrent colorectal cancer. cancer rectum prostate pubic bone bladder Small bowel
- 44. • CEA: High CEA levels associated with poorer survival • Routine investigation ▫ Complete blood count, RFT, LFT ▫ Chest X-ray
- 46. Surgery • Surgery is the mainstay of treatment of RC • Local recurrence after conventional surgery: ▫ 20%-50% (average of 35%)** • Radiotherapy significantly reduces the number of local recurrences
- 47. Types of Surgery • Local excision- reserved for superficially invasive (T1) tumors with low likelihood of LN metastases • Should be considered a total biopsy, with further treatment based on pathology • With unfavorable pathology patient should undergo total mesorectal excision with or without sphincter- preservation: ▫ positive margin (or <2 mm), lymphovascular invasion, ▫ poorly differentiated tumors, T2 lesion
- 48. • Low Anterior Resection - for tumors in upper/mid rectum; allows preservation of anal sphincter • Abdominoperineal resection ▫ for tumors of distal rectum with distal edge up to 6 cm from anal verge ▫ associated with permanent colostomy and high incidence of sexual and genitourinary dysfunction
- 49. Complications of Surgery • Bleeding • Infection • Anastomotic Leakage • Blood clots • Anesthetic Risks
- 51. Purpose of Radio(chemo)therapy in Rectal Cancer • To lower local failure rates and improve survival in resectable cancers • to allow surgery in primarly inoperable cancers • to facilitate a sphincter-preserving procedure • to cure patients without surgery: very small cancer or very high surgical risk
- 52. 5Fu Leucovorin Oxaliplatin Irinotecan Bevacizumab cetuximab Combinations FOLFOX FOLFIRI Leucovorin/5FU Capecitabine Bevacizumab in combination with the above regimens. Chemotherapy agents
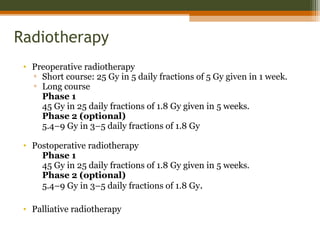
- 53. Radiotherapy • Preoperative radiotherapy ▫ Short course: 25 Gy in 5 daily fractions of 5 Gy given in 1 week. ▫ Long course Phase 1 45 Gy in 25 daily fractions of 1.8 Gy given in 5 weeks. Phase 2 (optional) 5.4–9 Gy in 3–5 daily fractions of 1.8 Gy • Postoperative radiotherapy Phase 1 45 Gy in 25 daily fractions of 1.8 Gy given in 5 weeks. Phase 2 (optional) 5.4–9 Gy in 3–5 daily fractions of 1.8 Gy. • Palliative radiotherapy
- 54. Clinical Trials
- 55. Pre-op RT vs. surgery alone Swedish Rectal Cancer Trial(NEJM 1997;336:980 ): 1168 patients randomised to 25 Gy (5x5) PRT or no RT. Surgery alone Preop. RT Rate of local recurrence 27% 11% p<0.001 5-year overall survival 48% 58% p=0.004 Dutch Colorectal Cancer Group (Kapiteijn E. NEJM 2001;345:638): 1861 patients randomised TME vs PRT+TME TME PRT+TME Recurrence rate 2.4% 8.2% OS ns ns
- 56. Pre-op vs. post-op Chemo RT Randomized trial of the German Rectal Cancer study Group (Sauer R et al. N Engl J Med 2004;351:1731-40): ▫ cT3 or cT4 or node-positive rectal cancer ▫ 50,4 Gy (1.8 Gy per day) ▫ 5-FU: 1000 mg/m2 per day (d1-5) during 1. and 5. week Preop CRT Postop CRT Patients N=415 N=384 5 y. OS 76% 74% p=0.8 5 y. local relapse 6% 13% p=0.006 G3,4 toxic effects 27% 40% p=0.001 • Increase in sphincter-preserving surgery with preop Th.
- 57. Thank You !!
Editor's Notes
- #58: There are interesting things to be found when researching information on the internet to include in a presentation. The Colossal Colon is a replica of the human colon that is four feet wide. It was modeled from colonoscopy footage. It has traveled across the U.S. to inform the public about colon health. People can crawl through the colon or view through windows on the outside. It shows healthy colon tissue as well as diseased tissue including polyps and colon cancer. This picture was taken at a mall near the Creighton University Medical Center. It’s a fun way to spread information about colon health.