Spinal anesthesia
- 1. SPINAL ANESTHESIA By : Dr. Vishal kr. kandhway
- 2. • Spinal anesthesia is also called as spinal block or subarachnoid block (sab). SAB is a regional anesthesia involving injection of a local anesthesia into the subarachnoid space which extends from the foramen magnum to S2 in adults and S3 in children. Injection of LA below LI in adults and L3 in children helps to avoid direct trauma to the spinal cord , (anesthetic agents acts on the spinal nerve and not on the substance of the cord)
- 3. Local Anesthetics used for Spinal Anesthesia • Procaine • Lidocaine • Mepivacaine • Tetracaine • Levobupivacaine • Bupivacaine
- 4. Short Acting Spinal Local Anesthetics • Procaine • Lidocaine • Mepivacaine Long Acting Spinal Local Anesthetics • Tetracaine • Bupivacaine • Ropivacaine • Levobupivacaine • Bupivacaine
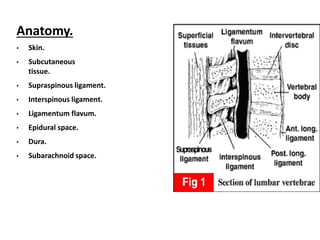
- 5. Anatomy. • Skin. • Subcutaneous tissue. • Supraspinous ligament. • Interspinous ligament. • Ligamentum flavum. • Epidural space. • Dura. • Subarachnoid space.
- 6. • The spinal cord usually ends at the level of L1 in adults and L3 in children. • Dural puncture above these levels is associated with a slight risk of damaging the spinal cord and is best avoided. • An important landmark to remember is that a line joining the top of the iliac crests is at L4 to L4/5
- 7. Mechanism of action: • Local anaesthetic solution injected into the subarachnoid space blocks conduction of impulses along all nerves with which it comes in contact, although some nerves are more easily blocked than others. • There are three classes of nerve: motor, sensory and autonomic. • Stimulation of the motor nerves causes muscles to contract and when they are blocked, muscle paralysis results.
- 8. • Sensory nerves transmit sensations such as touch and pain to the spinal cord and from there to the brain, whilst autonomic nerves control the caliber of blood vessels, heart rate, gut contraction. • Generally, autonomic and sensory fibers are blocked before motor fibres. This has several important consequences. For example, vasodilation and a drop in blood pressure may occur when the autonomic fibers are blocked. Practical implications of physiological changes. • The patient should be well hydrated before the local anaesthetic is injected and should have an intravenous infusion in place so that further fluids or vasoconstrictors can be given if hypotension occurs.
- 9. The Advantages of Spinal Anaesthesia: 1.Cost ( minimal ) 2.Patient satisfaction 3.Respiratory disease 4.Patent airway 5.Diabetic patients
- 10. Indications for Spinal Anaesthesia: • Spinal anaesthesia is best reserved for operations below the umbilicus e.g. hernia repairs, gynaecological and urological operations. • Any operation on the perineum or genitalia. • All operations on the leg are possible, but an amputation, though painless, may be an unpleasant experience for an awake patient.
- 11. • Older patients and those with systemic disease such as chronic respiratory disease, hepatic, renal and endocrine disorders such as diabetes. • It is suitable for managing patients with trauma if they have been adequately resuscitated and are not hypovolaemic. • In obstetrics, it is ideal for manual removal of a retained placenta (again, provided there is no hypovolaemia).
- 12. Contra-indications to Spinal Anaesthesia: Absolute: 1.Local site infection. 2.Coagulopathy or other bleeding disorders. 3.Shock 4.Patient refusal. 5.Increased Intracranial Pressure. 6.Severe aortic stenosis. 7.Severe Mitral stenosis. 8. Vertebral traumatic injuries 9. MI
- 13. Relative contraindication: 1.Sepsis 2.Uncooperative patients. Eg. Child, psyc pt. 3.Pre-existing neurological deficit. 4.Obese 5.Severe spinal deformities. 6.Intra-medullary tumor 7. Hypertension/hypotension 8. Prev. spine operated patients.
- 14. Bupivacaine (Marcaine). • 0.5% hyperbaric (heavy) bupivacaine is the best agent to use if it is available. • Bupivacaine lasts longer than most other spinal anaesthetics: usually 2-3 hours. Lignocaine (Lidocaine/Xylocaine). • Best results are obtained with 5% hyperbaric (heavy) lignocaine which lasts 45-90 minutes.
- 15. Cinchocaine (Nupercaine, Dibucaine, Percaine, Sovcaine). 0.5% hyperbaric (heavy) solution is similar to bupivacaine. Amethocaine (Tetracaine, Pantocaine, Pontocaine, Decicain, Butethanol, Anethaine, Dikain). A 1% solution can be prepared with dextrose, saline or water for injection. Mepivacaine (Scandicaine, Carbocaine, Meaverin). A 4% hyperbaric (heavy) solution is similar to lignocaine.
- 16. • Patients should be told about their anaesthetic during the pre-operative visit. • It is important to explain that although spinal anaesthesia abolishes pain, they may be aware of some sensation in the relevant area, but it will not be uncomfortable and is quite normal. • They must be reassured that, if they feel pain they will be given a general anaesthetic. Pre-operative Visit.
- 17. Premedication is not always necessary, but if a patient is apprehensive, 1. A benzodiazepine such as 5-10 mg of diazepam may be given orally 1 hour before the operation. 2. Other sedative or narcotic agents may also be used.
- 18. Pre-loading: • All patients having spinal anaesthesia must have a large intravenous cannula inserted and be given intravenous fluids immediately before the spinal. • The volume of fluid given will vary with the age of the patient and the extent of the proposed block. • A young, fit man having a hernia repair may only need 500 ml • Older patients are not able to compensate as efficiently as the young for spinal-induced vasodilation and hypotension and may need 1000ml for a similar procedure. • If a high block is planned, at least a 1000ml should be given to all patients. • Caesarean section patients need at least 1500 ml.
- 19. The fluid should preferably be normal saline or ringer lactate. 5% dextrose is readily metabolised and so is not effective in maintaining the blood pressure.
- 20. Position: 1.Lateral ( Left or Right lateral ) 2.Sitting
- 21. • Males tend to have wider shoulders than hips and so are in a slight "head up" position when lying on their sides, • whilst for females with their wider hips, the opposite is true.
- 23. SITTING POSITION
- 24. • The sitting position is preferable in the obese whereas • The lateral is better for uncooperative or sedated patients.
- 25. How to perform the spinal injection? • Clean the patient’s back with antiseptic. • Locate a suitable interspinous space. • Raise an intradermal wheal of LA agent at proposed puncture site.
- 27. How to perform the spinal injection? Insert the needle: the structures that will be passed skin , subcutaneous tissue, supraspinous ligament , interaspinous ligament , lagementum flavum , dura mater. When CSF appears then slowly inject the local anesthetic.
- 28. 28
- 29. Factors affecting the spread of local anesthetic solutions in CSF 1. The baricity of the local anesthetic solution. 2. The position of the patient . 3. The level of injection. 4. The speed of injection ( like all anesthetics ). 5. Obesity : as increase in intra-abdominal pressure decreases the subarachnoid space so doses must be reduced. 6. Pregnancy : increase in intra-abdominal pressure leading to increase in peridural veins filling leading to less subarachnoid space and less doses.
- 30. Complication: 1.Immediate complication: - Hypotension and Cardiac arrest. - Total spinal block leading to respiratory arrest. - bradycardia - nausea/vomiting, Bleeding, failure of spinal anesthesia. 2.Late complication: - Post dural puncture headache (PDPH) - Backache - urinary retension - Bacterial meningitis/radiculopathy/shievering.
- 31. 4Treatment of Hypotension. • Hypotension is due to vasodilation and a functional decrease in the effective circulating volume. 1.vasoconstrictor drugs 2.All hypotensive patients should be given OXYGEN by mask until the blood pressure is restored. 3. Raising their legs thus increasing the return of venous blood to the heart. .Increase the speed of the intravenous infusion to maximum until the blood pressure is restored to acceptable levels. 5. pulse is slow, give atropine intravenously.
- 32. • It is widely considered that pencil-point needles (Whiteacre or Sprotte) make a smaller hole in the dura and are associated with a lower incidence of headache (1%) than conventional cutting-edged needles (Quincke)
- 34. Treatment of spinal headache. 1.Remain lying flat in bed as this relieves the pain. 2.They should be encouraged to drink freely or, if necessary, be given intravenous fluids to maintain adequate hydration. 3.Simple analgesics such as paracetamol, aspirin or codeine may be helpful,
- 35. 4.Caffeine containing drinks such as tea, coffee or Coca- Cola are often helpful. 5. Prolonged or severe headaches may be treated with epidural blood patch performed by aseptically injecting 15-20ml of the patient's own blood into the epidural space. This then clots and seals the hole and prevents further leakage of CSF. It used to be thought that bedrest for 24 hours following a spinal anaesthetic would help reduce the incidence of headache.