Common pitfalls in bone marrow biopsy based diagnostic approach
- 1. Common pitfalls in bone marrow biopsy based diagnostic approach Dr. N. Varma Prof. & Head - Hematology PGIMER, Chandigarh, India
- 2. Bone marrow (BM) examination • Gold standard investigation for diagnosing and monitoring many hematological diseases • Useful for investigating various non-hematological conditions • Combination of bone marrow aspirate and trephine biopsy: fine cytological detail, the organization of BM, and the presence of focal abnormalities
- 3. Good-to-have Information • Accurate clinical information; context and questions being asked; details of previous investigations • For neoplastic diseases: ? primary diagnostic investigation/ staging procedure/ re-examination to assess response to treatment (including transplantation) • The type and timing of previous BM transplantation are also important factors; kinetics of engraftment differ between conditioning regimes and graft types • Knowledge of the recent therapeutic use of growth factors such as G-CSF; these may transiently have major modifying effects on hemopoiesis that can mask or mimic genuine pathology
- 4. Pitfalls in obtaining and interpreting bone marrow aspirates • BM aspiration done when not needed • BM aspiration not done when needed • BM aspiration done on the wrong site • The clinical context not adequately assessed and the correct range of tests is therefore not done on the aspirate • False negative result as a consequence of a sampling error • The aspirate is not interpreted together with the trephine biopsy sections • The aspirate is misinterpreted – Problems relating to technical quality – Correct stains not performed – Features present not noted – Misinterpretation of an adequate aspirate
- 5. Limiting factors for interpretation of BMB • Inadequate clinical, hematological (blood and aspirate findings), genetic and radiological information • Inadequate specimen – Too small – Too crushed/distorted – Both – Poorly decalcified/processed • Inadequate sections (thickness, number of levels) • Inadequate stains (poor technical quality, range too limited) • Insufficient experience to avoid common pitfalls (eg, differential diagnosis of granulomas or fibrosis) • Insufficient confidence to avoid concluding ‘consistent with’ • ‘Invisible’ pathology • Forgetting to look at the bone trabeculae and stroma
- 6. Common Ancillary Studies complementary to Bone Marrow Morphologic Examination • Cytogenetics on BM aspirate or peripheral blood sample • FISH studies on BM aspirate or touch preparations • Molecular studies (PCR or RT-PCR) to detect specific translocations and/or antigen receptor gene rearrangements • Flow cytometric Immunophenotyping of BM aspirate or peripheral blood cells • Immunohistochemistry on paraffin sections • Enzyme cytochemistry on marrow aspirate or peripheral smear slides
- 7. A systematic approach to diagnosis is required for: • D/D of hypoplasia/aplasia • D/D of megaloblastic hemopoiesis • Assessing key histological features of myelodysplastic and myeloproliferative haemopoiesis • D/D of bone marrow fibrosis • Assessing patterns of lymphoid infiltration associated with various lymphomas, especially small B-cell lymphomas • D/D of granulomatous pathologies
- 8. 1. D/D hypocellular marrow Normocellular
- 9. • CBC and reticulocyte count • Blood film examination • Bone marrow aspirate and trephine biopsy • HbF% in children • Peripheral blood lymphocyte cultures for clastogens induced chromosomal breakage studies • Ham’s test and / or flowcytometry for GPI anchored proteins • Urine hemosiderin (if Ham’s test and / or FCM for GPI anchored +) • Vitamin B12 and folate levels • Liver function tests • Renal function tests • Viral markers (hepatitis A, B, C; EBV; CMV; HIV) • Antinuclear antibody and anti ds-DNA • Chest x-ray • Abdominal ultrasound scan Investigations recommended for suspected AA
- 10. CBS 958 Varma N et al. Multiple constitutional aetiological factors in BMFS patients… Indian J Med Res 2006 Fanconi Anemia associated Aplastic Anemia
- 11. (A-1366/11; Tx-1204/11) 2. Subtle increase of immature cells: in hypocellular marrow ?leukemia/lymphoma
- 12. IHC: Blasts positive for CD34, anti-MPO (A-1366/11; Tx-1204/11) Diagnosis: Hypocellular AML 2. Subtle increase of immature cells in hypocellular marrow
- 13. 3. Problem in differentiating AML-M6 and megaloblastic anemia Megaloblastic anemia ? Megaloblastic anemia
- 14. 3. Problem in differentiating AML-M6 and megaloblastic anemia (A-1305/10; Tx-1056/10) IHC: Blasts positive for anti-MPO, CD34 AML- M6
- 15. Hb TLC Platelet count Reticulocyte DLC PBF 7 g/dl 7.3 x 109/L 7 x 109/L 5.36% P60L34M4E2 Moderate anisocytosis, microcytes, macrocytes, hypochromia & polychromasia 3. D/D of ‘megaloblastic anemia’ picture
- 16. Bone marrow aspirate (BM A-1404/12) Cellular M:E= 1:1 Blast1, Pm2, My 40 ,Mm 1, P44, L8, M1, E2 Megakaryocytes: Adequate
- 17. Bone marrow biopsy (T-1226/12) Mildly hypercellular with relative erythroid hyperplasia with megaloblstic changes. Granulocytes and megakaryocytes are adequate.
- 19. Granulocytes
- 20. Granulocytes
- 21. Monocytes
- 22. RBCs Final diagnosis: Classical PNH
- 23. RCMD-RS 3. D/D of ‘megaloblastic anemia’ picture: characterization of ‘MDS’ like pathology. 45 M, bicytopenia
- 24. Bone marrow infiltration in a case of Hepatosplenic lymphoma (A-408/10; Tx-323/10) 4. Pattern of bone marrow infiltration by NHL
- 25. Bone marrow intravascular infiltration in a case of Hepatosplenic lymphoma. IHC for CD34 and CD3 (A-408/10; Tx-323/10) CD34 CD3 4. Pattern of bone marrow infiltration by NHL
- 26. Plasma cells in a case of Multiple myeloma (A-1441/08; Tx-1161/08) 5. Differentiation between reactive and malignant plasma cells IHC: Kappa light chain
- 27. Reactive plasmacytosis + LD bodies (A-1535/11; Tx-1356/11) 5. Differentiation between reactive and malignant plasma cells
- 28. Reactive increase in plasma cells in a case of Tubercular Granuloma (A-1198/12; Tx-1042/12) 5. Differentiation between reactive and malignant plasma cells
- 30. Renal Osteodystrophy (A-391/12; Tx-339/12) 6. Identification of etiology in fibrosis
- 31. 6. Identification of etiology in fibrosis Acute panmyelosis with myelofibrosis (A-185/13; Tx-167/13)
- 32. ALL with fibrosis (A-1476/12; Tx-1288/12) 7. Identification of subtle infiltration of leukemia/lymphoma in fibrotic marrow
- 33. IHC for CD34 7. Identification of subtle infiltration of leukemia/lymphoma in fibrotic marrow; IHC is required IHC for TdT IHC for CD20 ALL with fibrosis (A-1476/12; Tx-1288/12)
- 34. Amyloid deposition in vessel wall (A-1554/12; Tx-1356/12) Congo Red stain 8. Problem in cases with subtle Amyloid deposition- need to be confirmed by special staining by Congo Red
- 35. 9. Problem in assigning myelodysplasia as reactive or primary RCMD- predominantly dysplastic megakaryocytes (A-803/12; Tx-690/12)
- 36. 9. Problem in assigning myelodysplasia as reactive or primary Case with sepsis- dysplastic megakaryocytes (A-55/12; Tx-51/12)
- 37. Metastatic carcinoma of GIT (A-105/13; Tx-93/13) 10. Problem in assessment of focal lesions- like metastasis may be missed if sample is inadequate, and also in identification of primary site. These non- hematologic malignancies may mimic hematological malignancies also.
- 38. Metastatic carcinoma- Prostate (A-983/09; Tx-763/09) 10. Problem in assessment of focal lesions- like metastasis may be missed if sample is inadequate, and also in identification of primary site. These non- hematologic malignancies may mimic hematological malignancies also.
- 39. Granuloma- TB (A-1198/12; Tx-1042/12) 11. Problem in assessment of focal lesions- like granuloma may be missed if inadequate sample and also in differentiation of granuloma etiology
- 40. Granuloma- Hodgkin’s Lymphoma (A-1252/12; Tx-1091/12) 11. Problem in assessment of focal lesions- like granuloma may be missed if inadequate sample and also in differentiation of granuloma etiology
- 41. 12. Problem in cases with only necrosis- where etiology can not be assessed BM Necrosis- (A-330/11; Tx-286/11)
- 42. 13. Problem in identification of lymphocytosis, esp in NK/ T-cell infiltration as reactive increase or malignant NK leukemia/lymphoma (A-444/12; Tx-314/12)
- 43. Bone Marrow Trephine Biopsy 314/12 Splenectomy section (S-12985/12) of this case. IHC for CD56 highlighting NK cell increase in spleen; case with increased lymphocytes on bone marrow. 13. Problem in identification of lymphocytosis, esp in NK/ T-cell infiltration as reactive increase or malignant
- 44. 14. Problem in differentiation of syntitial variant of Hodgkin’s lymphoma and ALCL Reported as Anaplastic large cell lymphoma (A-1255/08; Tx-1020/08)
- 45. IHC for CD30 IHC for CD15 14. Problem in differentiation of syntitial variant of Hodgkin’s lymphoma and ALCL- IHC required for differentiation Reported as Anaplastic large cell lymphoma (A-1255/08; Tx-1020/08)
- 46. 15. Problem in identification T-cell rich B-cell lymphoma IHC for CD3 IHC for CD20
- 47. 16. There can be technical artefacts leading to inconclusive findings Washed off marrow spaces
- 48. Washed off marrow spaces, hemorrhage and cartilage 16. Procedural artefacts leading to inconclusive findings
- 49. 16. Technical artefacts leading to inconclusive findings Crushed marrow spaces
- 50. 17. 15yrs/M, TLC 32x109/L, Blasts 95% Scanty aspirate smears Tx BxPB smear MPO +
- 51. Positive Markers: CD13, CD33, Anti MPO, CD19, CD10, CD34, CD45, CD123, H LADR Negative Markers: T lineage FCM-IP Diagnosis: Mixed Phenotype Acute Leukemia (B/ Myeloid)
- 52. 1444 bp 943 bp 754 bp 585 bp 458 bp 341 bp 258 bp NC P1 P2 P3 P4 P5 P6 M bcr-abl transcripts in 1 MPAL (P1) and 5 different CML (P2-6) patients b3a2 – 385 bp b2a2 – 310 bp Bhatia P, Binota J, Varma N, Bansal D, Trehan A, Marwaha RK, Malhotra P, Varma S. A Study on the Expression of BCR-ABL Transcript in Mixed Phenotype Acute Leukemia (MPAL) Cases Using the Reverse Transcriptase Polymerase Reaction Assay (RT-PCR) and its Correlation with Hematological Remission Status Post Initial Induction Therapy. Mediterr J Hematol Infect Dis. 2012;4(1):e2012024.
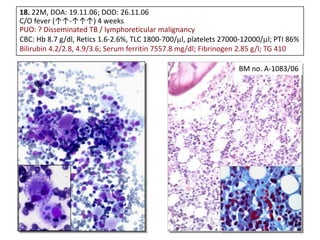
- 53. 18. 22M, DOA: 19.11.06; DOD: 26.11.06 C/O fever (↑↑-↑↑↑) 4 weeks PUO: ? Disseminated TB / lymphoreticular malignancy CBC: Hb 8.7 g/dl, Retics 1.6-2.6%, TLC 1800-700/ l, platelets 27000-12000/ l; PTI 86% Bilirubin 4.2/2.8, 4.9/3.6; Serum ferritin 7557.8 mg/dl; Fibrinogen 2.85 g/l; TG 410 BM no. A-1083/06
- 54. EBV Zebra LMP 1 EBNA HPS / HLH •Screen for underlying genetic, autoimmune, infectious and malignant diseases •Uncontrolled hypercytokinemia & many triggers •Early diagnosis and Rx PM no. 21703
- 55. 19. 5 ys. FCh; AML with increased mast cells/ basophils
- 57. P 30 / 07: CD 117 (APAAP) Varma N, Varma S, Wilkins B. Br J Haematol 2000;111:991. Mast cell tryptase AML with mastocytosis [Systemic mastocytosis with associated clonal hematological non-mast cell disease (SM-AHNMD)]
- 58. Few representative examples • Assessment of focal lesions • Differentiation between reactive lymphoid infiltrate and NHL • Differentiation between reactive and malignant plasma cells • Identification of malignancies with associated fibrosis • Effect of growth factors • Differentiation between hematogones and blasts • Differentiation between megaloblastic anemia and acute leukemia • Differentiation between aplastic bone marrow and hypoplastic myelodysplastic syndrome or hypoplastic acute leukemia • Identification of lymphomas having a tendency for intravascular infiltration in the BM • Subtle amyloid deposition • Differentiation of macrophage infiltrates and other pathologies that resemble granulomatous infiltration • Procedure related artefacts
- 59. Take home message • Integration of clinical, laboratory and imaging information • Not to assess histology in isolation; uni- / bilateral bx; dry aspirate • Components of an integrated approach to interpretation are: – Adequate size of trephine core, with minimal disruption by trauma caused during collection. – Access to detailed clinical information and results of additional tests (specially, peripheral blood cell counts, blood and BM aspirate cytomorphology, flow cytometry, cytogenetic analysis and radiological imaging). – Systematic assessment of all BM components, including trabecular bone and interstitial stroma. – Awareness of pathologies that may be ‘invisible’ in trephine specimens without immunostaining. – Use of preselected antibody panels for immunostaining and familiarity with the expected results, including controls. – Experience in interpreting additional molecular studies, such as clonality PCR and fluorescence in-situ hybridization. – Familiarity with the major patterns of bone marrow involvement by reactive and neoplastic conditions and their differential diagnosis. – A collaborative approach to working with diverse clinical and laboratory colleagues. – Ideally, hematopathologists should report BM Bx along with BM aspirate.
- 60. Thank You Common pifalls in BMB interpretation can be avoided
Editor's Notes
- #61: Contribute to diagnose and treat AMLs better!























































![P 30 / 07: CD 117 (APAAP)
Varma N, Varma S, Wilkins B.
Br J Haematol 2000;111:991.
Mast cell tryptase
AML with mastocytosis [Systemic mastocytosis with associated
clonal hematological non-mast cell disease (SM-AHNMD)]](https://image.slidesharecdn.com/01commonpitfallsofbmb-nvarma-130823174915-phpapp02/85/Common-pitfalls-in-bone-marrow-biopsy-based-diagnostic-approach-57-320.jpg)


